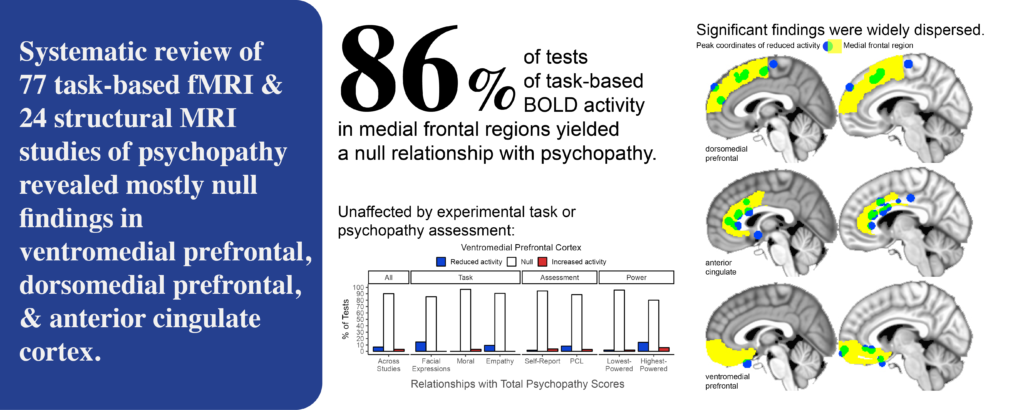
For decades, scientists have thought the medial frontal cortex may play a critical role in psychopathy. We put this hypothesis to the test by gathering the findings from 101 MRI studies.
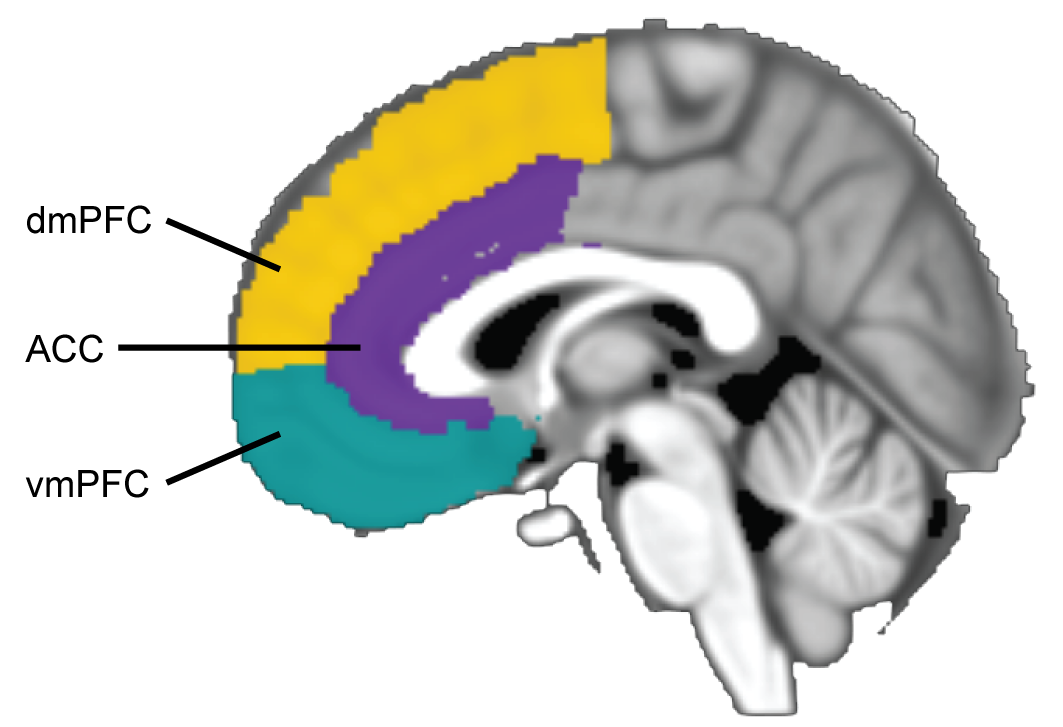
To be clear, we’re talking about the region directly behind the bridge of your nose and the center of your forehead, going up nearly to the top of your head. It’s medial – meaning towards the middle – and frontal – which translates roughly to ‘frontal.’ And it’s the cortex – the outer layer of gray matter in the brain.
Let’s break the medial frontal cortex up into three regions: the ventromedial prefrontal cortex (vmPFC), anterior cingulate cortex (ACC), and dorsomedial prefrontal cortex (dmPFC). See the diagram below. Now, we could (and probably should) break these three regions up even further (based on things like the organization of cells in each region). But we can focus on these three regions, because that’s mainly what scientists studying psychopathy have done.
The vmPFC, in particular, has been linked to psychopathy for a long time – or at least to behaviors that resemble psychopathy. You may know the famous case of Phineas Gage. In 1848, Gage was constructing a railroad when an explosion blasted a metal rod through his skull. Miraculously, Gage survived the accident. But the blast permanently damaged his vmPFC and other frontal brain tissue. Afterwards, friends of Gage said his personality changed. He was now unreliable, impulsive, and vulgar – traits that in part resemble psychopathy. More than a century later, scientists would name the behavior changes that tend to follow vmPFC damage: ‘acquired sociopathy’ or ‘pseudopsychopathy.’
There’s a lot of research showing that vmPFC and ACC are involved in emotion, empathy, and decision-making, while dmPFC is involved in thinking about oneself and other people. So, researchers made a hypothesis: lower activity and volume in medial frontal cortex (especially vmPFC and ACC) cause psychopathic people’s shallow emotions, callousness towards others, and impulsive decision-making.
It has been 20 years since researchers made this hypothesis, and in that time 101 MRI studies have tested the relationship between psychopathy and medial frontal cortex.
What does the data say?
Unfortunately, as we found out, by far the most common finding was that psychopathy and medial frontal cortex were unrelated.
In the 101 MRI studies, we counted 1,322 individual tests of activity – meaning researchers tested the relationship between psychopathy and medial frontal activity 1,322 times. In 86% of these tests, psychopathic people and relatively healthy people showed similar medial frontal activity.
We also counted 251 individual tests of volume. In 83% of these tests, psychopathic people and relatively healthy people showed similar medial frontal volume.
Let’s zoom in on one of the medial frontal regions, the ACC. In the graph below, you can see the percentage of studies that found reduced ACC activity (in blue) or increased ACC activity (in red) among psychopathic people. You can also see the percentage of studies that found similar ACC activity (in white) among psychopathic compared to relatively healthy people. From now on I’ll call these findings – where psychopathy and ACC activity are unrelated – ‘null.’
On the far left, you can see the results for all studies. Most studies reported at least one null test. Far fewer studies reported reduced or increased ACC activity.
This was true regardless of the study’s experimental task, method of assessing psychopathy, or power (sample size), as you can see above.
Although, you’ll notice that using an empathy task made null findings slightly less likely, and made findings of altered activity more likely. It’s noteworthy that null findings were still the most common. And, these studies observed reduced activity and increased activity at similar rates. So the findings were inconsistent. Lastly, of the nine studies that used an empathy task, three studies (which found altered activity) came from the same research group and included overlapping samples of participants. For these reasons, I’m avoiding drawing strong conclusions about empathy tasks.
What about the findings of altered activity? Were they in similar locations? No: as you can see below, they were widely scattered.
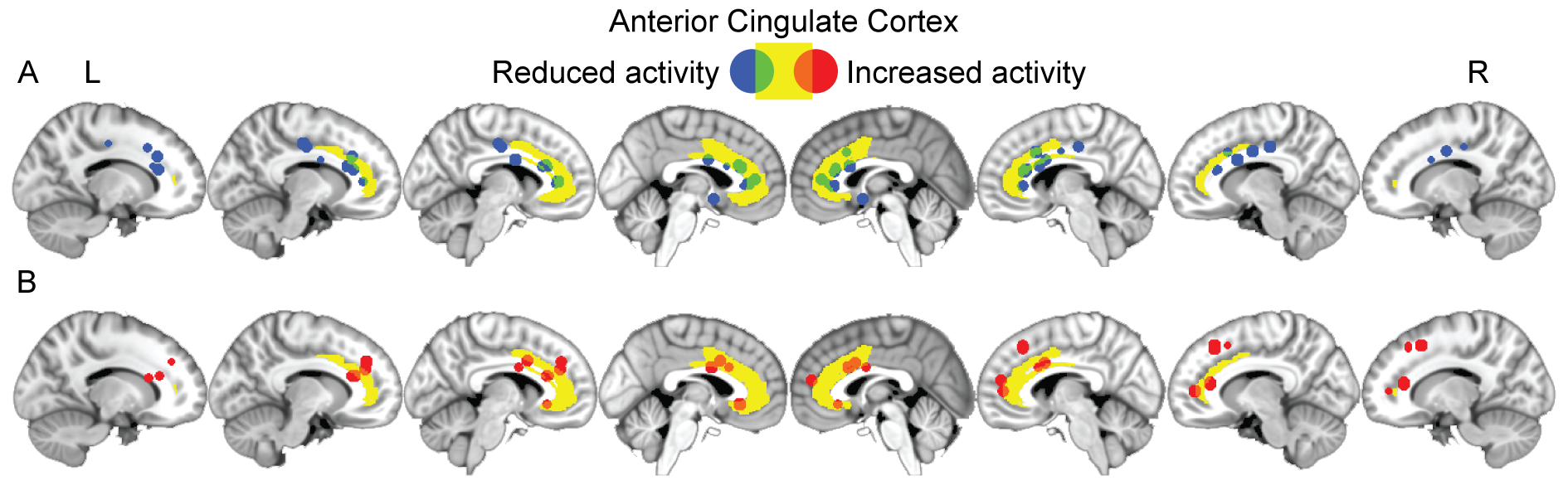
For each finding of altered activity, we pulled out the ‘peak coordinates,’ which tell us the point at which the relationship with psychopathy was greatest. Above, you can see that the peak coordinates (in blue/green) where psychopathic people showed reduced ACC activity were widely scattered. Most of these peak coordinates did not fall within the ACC (in yellow). The same was true for the peak coordinates where psychopathic people showed increased activity (in red/orange).
We found this same pattern of results for the vmPFC and dmPFC as well. If you’re interested, you can see those results in the full paper. The link is at the bottom of this page.
So, to recap:
Psychopathy was rarely related to medial frontal activity or volume.
Among the findings of altered activity, there was a lot of inconsistency. Some tests found reduced activity, others increased activity. Few tests found altered activity in the same place.
Here are a few ideas to take away from this study.
- We think it’s time to update our theories and methods to address these null and heterogeneous findings. For starters, we should consider the possibility that there is no consistent ‘neural profile’ of psychopathy. Instead, brain disruptions may be unique to each person.
- There is scant evidence that psychopathy is related to disruptions in any of the most theoretically relevant brain regions: the vmPFC, ACC, or amygdala.
- The lack of consistency in MRI studies is not just a problem in the field studying psychopathy. Inconsistent MRI findings have accumulated for virtually all mental illnesses.
- If there is a ‘neural profile’ of psychopathy, I think we’re most likely to find it at the level of large-scale brain networks. Other scientists and I have found disruptions in two networks in particular, the default mode and salience networks.
- We cannot and do not use MRI to diagnose psychopathy. We have plenty of clinical interviews and questionnaires for diagnosis.
- Our findings raise serious concerns about using MRI evidence to inform decisions in legal settings.
Read the full paper here.
Deming, P., Griffiths, S., Jalava, J., Koenigs, M., & Larsen, R.L. (2024). Psychopathy and medial frontal cortex: A systematic review reveals predominantly null relationships. Neuroscience & Biobehavioral Reviews, 167, 105904.